How to Diagnose Infertility in Females?
Infertility is a growing concern for many couples worldwide, with approximately 10-15% of couples facing challenges in conceiving. Female infertility contributes to nearly half of these cases and can arise due to various medical, genetic, or lifestyle-related factors. Proper diagnosis is crucial to understand the underlying causes and to explore effective solutions, such as female infertility treatment in Kenya, where specialized care and advanced medical interventions are available.
In this article, we’ll discuss the various methods used to diagnose female infertility, including medical history evaluation, physical examinations, and diagnostic tests, and how these steps pave the way for effective treatment.
Understanding Female Infertility
Female infertility refers to the inability to conceive after trying for 12 months or more of unprotected sexual intercourse. For women over the age of 35, this duration is reduced to six months due to age-related declines in fertility. Causes can range from hormonal imbalances and structural abnormalities to lifestyle choices or unexplained factors.
Steps to Diagnose Female Infertility
1. Comprehensive Medical History
The first step in diagnosing female infertility is a thorough evaluation of the patient’s medical history. This includes:
- Menstrual Cycle History: Questions about irregular, absent, or painful periods may provide insights into ovulatory dysfunction.
- Past Pregnancies: A history of previous pregnancies, miscarriages, or ectopic pregnancies helps assess reproductive health.
- Medical Conditions: Conditions such as polycystic ovary syndrome (PCOS), endometriosis, or thyroid disorders are closely examined.
- Surgical History: Past surgeries involving the abdomen, pelvis, or reproductive organs can affect fertility.
- Lifestyle Factors: Smoking, alcohol consumption, weight issues, and stress levels are evaluated, as they can impact fertility.
2. Physical Examination
A physical examination by a gynecologist or fertility specialist can help detect signs of underlying conditions:
- Pelvic Exam: This involves checking for abnormalities in the reproductive organs, such as ovarian cysts, fibroids, or uterine irregularities.
- Body Mass Index (BMI): BMI is assessed, as being overweight or underweight can disrupt hormone levels and ovulation.
- Signs of Hormonal Imbalance: Unusual hair growth, acne, or breast discharge may indicate endocrine issues.
3. Ovulation Assessment
Ovulation is a key factor in female fertility. Tests to determine ovulation include:
- Basal Body Temperature (BBT) Tracking: Women record their daily body temperature to identify slight increases that occur during ovulation.
- Ovulation Predictor Kits (OPKs): These kits detect luteinizing hormone (LH) surges in urine, indicating ovulation.
- Progesterone Test: A blood test measures progesterone levels, which rise after ovulation.
4. Hormonal Testing
Hormonal imbalances are a common cause of female infertility. Blood tests are used to evaluate the levels of critical hormones, including:
- Follicle-stimulating hormone (FSH): Indicates ovarian reserve and the ability to produce eggs.
- Luteinizing Hormone (LH): Helps identify ovulatory disorders.
- Estrogen and Progesterone: Assess the menstrual cycle’s health.
- Anti-Müllerian Hormone (AMH): Measures ovarian reserve and the remaining egg supply.
- Thyroid Hormones (TSH): Thyroid dysfunction can disrupt ovulation and menstruation.
5. Imaging Tests
Imaging techniques are used to visualize the reproductive organs and identify structural abnormalities. Common imaging tests include:
- Ultrasound: A pelvic ultrasound evaluates the uterus, ovaries, and fallopian tubes for abnormalities like cysts, fibroids, or blocked tubes.
- Hysterosalpingography (HSG): An X-ray procedure examines the uterus and fallopian tubes by injecting a contrast dye. It helps detect blockages or structural issues in the tubes.
- Sonohysterography: This test involves using saline and ultrasound to provide detailed images of the uterine cavity.
- Magnetic Resonance Imaging (MRI): For complex cases, an MRI offers a comprehensive view of reproductive anatomy.
6. Genetic Testing
In cases where the cause of infertility is unclear or there’s a history of recurrent pregnancy loss, genetic testing may be recommended. This helps identify chromosomal abnormalities or genetic conditions that may affect fertility.
Preparing for the Diagnosis Process
The journey to diagnosing female infertility can be emotionally and physically demanding. Preparing mentally and physically is important:
- Maintain a Healthy Lifestyle: Eating a balanced diet, exercising regularly, and managing stress can improve overall health and fertility.
- Partner Involvement: Both partners should undergo evaluations, as male factors contribute to infertility in about 30% of cases.
- Stay Informed: Understanding the diagnostic process and potential treatments can empower you to make informed decisions.
Conclusion
Diagnosing female infertility involves a combination of medical history evaluation, physical exams, and advanced diagnostic tests to identify the root cause. For couples seeking solutions, female infertility treatment in Kenya provides access to cutting-edge diagnostic tools and treatments, guided by experienced fertility specialists. Early diagnosis and intervention can significantly improve the chances of conception, paving the way for parenthood and a fulfilling family life. By addressing infertility with a proactive approach, women can find hope and success in their fertility journey.
FAQ's
What causes infertility in women?
Infertility can result from hormonal imbalances, blocked fallopian tubes, ovulation disorders, endometriosis, or age-related factors. Lifestyle habits and underlying medical conditions may also affect fertility. Accurate diagnosis helps determine effective treatment options.
How is female infertility diagnosed?
Doctors diagnose infertility through medical history, physical exams, hormone tests, ovulation tracking, ultrasound scans, and imaging of reproductive organs. In some cases, laparoscopy is used to check for conditions like endometriosis or blocked tubes.
When should I see a doctor for infertility?
You should see a fertility specialist if you’ve tried to conceive for over a year (or six months if over 35) without success. Early evaluation helps identify causes and improves chances of successful conception.
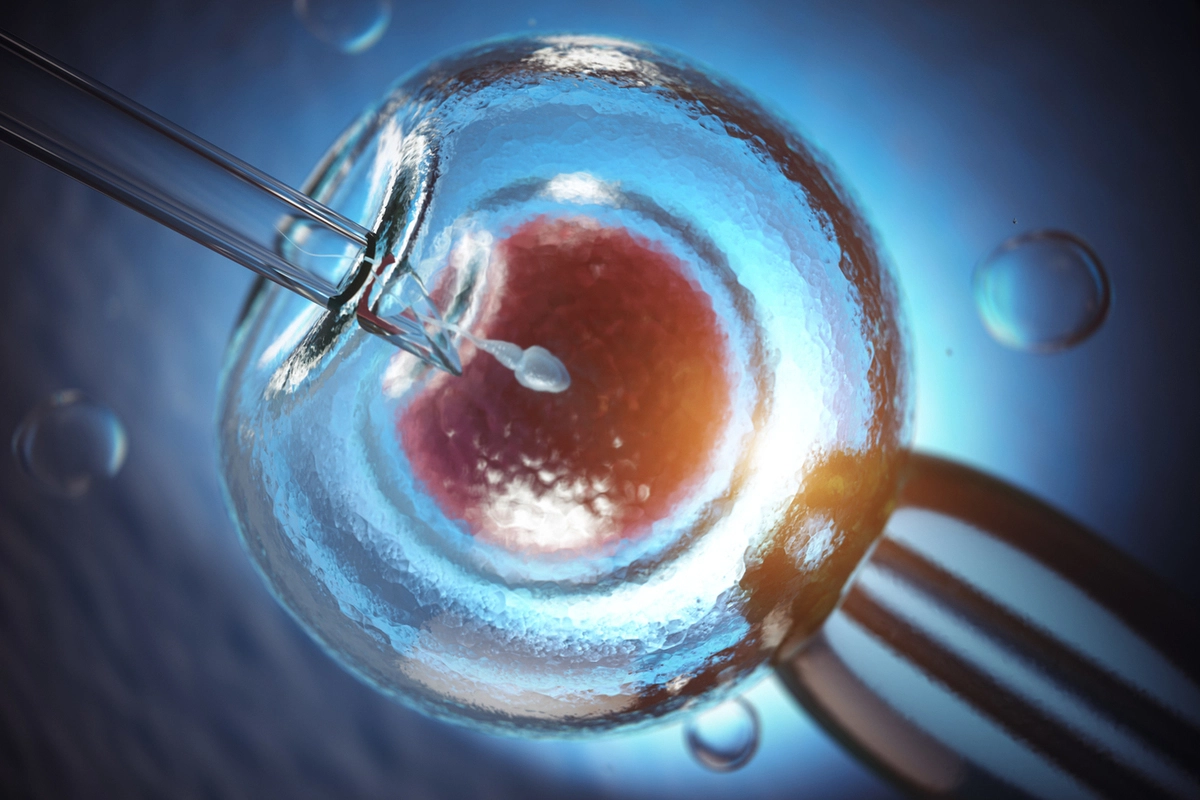
Can infertility in women be treated?
Yes. Treatment depends on the cause and may include medication for ovulation, hormone therapy, surgery to correct structural problems, or assisted reproductive technologies like IVF. Early diagnosis and proper care greatly improve success rates.