Male Infertility Reasons: Common Causes, Signs, and Treatment Paths

Hearing that tests point to a male factor can feel like the floor has dropped away. Many people still picture infertility as a “women’s problem,” yet male infertility contributes to about half of all cases where a couple has trouble conceiving.
Research suggests that up to 7% of men face fertility challenges. That makes this a common medical issue, not a rare exception. It is not a sign of weakness or masculinity being “less than.” It is a health condition that can often be explained and treated.
Understanding the main male infertility reasons is the first practical step toward change. Once a likely cause is identified, treatment options become clearer—from lifestyle adjustments to advanced procedures such as IVF (in vitro fertilization) and ICSI (intracytoplasmic sperm injection).
Fertility Point builds on these medical advances with modern diagnostics, experienced specialists, and ongoing emotional support for both partners. The team focuses on clear assessment, honest discussion, and treatment plans that match each couple’s situation.
By the end of this article, you’ll know what male infertility means, how common it is, how to spot warning signs, which medical and lifestyle factors matter most, and which treatment paths clinics like Fertility Point can offer.
Understanding Male Infertility: What It Means And How Common It Is

Male infertility is a condition where problems in the male reproductive system make it difficult or impossible to achieve pregnancy with a fertile partner. Doctors usually start investigating if a couple has regular, unprotected sex for 12 months without conceiving (or 6 months if the female partner is 35 or older).
Male factors are involved in about 50% of infertility cases, either on their own or together with female factors.
“Infertility is a disease of the reproductive system defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse.” — World Health Organization (WHO)
It helps to separate fertility from identity. A low sperm count, hormone issues, or blocked ducts say nothing about a man’s strength or character. They indicate that one body system isn’t working as well as it could—just like high blood pressure or diabetes.
Many male infertility causes are manageable. A full check?up can reveal:
-
Varicocele (enlarged veins around the testicle)
-
Past or current infections
-
Hormonal or genetic issues
-
Blockages in the sperm pathway
-
Lifestyle and environmental factors
Often, the first and only sign is difficulty conceiving. Some men also notice changes in sexual function, testicular appearance, or body hair. A structured assessment at a clinic such as Fertility Point pulls these clues together into a clear picture and guides the next steps.
Recognizing The Signs And Symptoms Of Male Infertility
For many men, the only obvious sign is that pregnancy is not happening. That alone is enough reason to seek a fertility evaluation. Still, certain symptoms can act as earlier warning signs.
Doctors commonly group them into three areas:
-
Problems with sexual function
-
Changes in the testicles or scrotum
-
Wider hormonal or physical indicators
Sexual Function Challenges
Sex and fertility rely on healthy blood flow, nerves, and hormones. Problems here can affect the ability to have intercourse or deliver sperm where it needs to go.
Typical issues include:
-
Difficulty getting or keeping a firm erection
-
Problems with ejaculation (very little semen, delayed ejaculation, or “dry” orgasm)
-
Noticeable drop in sex drive
These signs can reflect hormone imbalance, nerve damage, medication side?effects, or other health conditions. Specialists at Fertility Point assess these symptoms with sensitivity and can suggest treatments that support both sexual function and fertility.
Physical Signs In The Testicular Area
The testicles need a good blood supply, a slightly cooler temperature than the rest of the body, and an open pathway for sperm. Warning signs in this area can include:
-
Pain, swelling, or a lump in the scrotum
-
A feeling of heaviness or dragging
-
Enlarged, twisted veins that look like a “bag of worms” (often a varicocele)
-
Testicles that look smaller or seem to have shrunk
New pain, lumps, or changes in size or firmness should be checked promptly. Because testicles produce both sperm and testosterone, Fertility Point advises men to seek medical care quickly for any unusual finding here.
Hormonal And Physical Indicators
Hormones from the brain, thyroid, and adrenal glands help control sperm production and sexual function. When they’re out of balance, changes can show up across the body, such as:
-
Breast enlargement in men (gynecomastia)
-
Loss or thinning of facial or body hair
-
Low energy, low mood, or reduced muscle mass
-
In some genetic conditions, repeated chest or sinus infections, or a poor sense of smell (anosmia)
These patterns may not be obvious to the person experiencing them, but experienced fertility doctors recognize them as clues. At Fertility Point, hormone tests and a careful physical exam help connect these signs to possible underlying causes.
Medical Causes Of Male Infertility
Many medical conditions can reduce sperm production or block sperm from reaching the ejaculate. Common groups include:
-
Varicocele
-
Infections and inflammation
-
Hormonal and endocrine disorders
-
Cancer and its treatments
-
Autoimmune reactions
Varicocele: The Leading Reversible Cause
A varicocele is an enlargement of the veins inside the scrotum, similar to varicose veins in the legs. It is one of the most frequent findings in men with abnormal semen tests. Extra warm blood in these veins can:
-
Raise testicular temperature
-
Reduce sperm count
-
Worsen sperm motility and shape
Symptoms may include dull ache, heaviness, or visible twisted veins. A microsurgical procedure called varicocelectomy ties off the enlarged veins while preserving important vessels. At Fertility Point, many men see better semen quality within a few months of surgery, and some couples conceive naturally afterward.
Infections And Inflammatory Conditions
Infections in the reproductive tract can damage the delicate structures where sperm are made and stored. Key examples:
-
Epididymitis (inflammation of the epididymis)
-
Orchitis (inflammation of the testicle), sometimes after mumps
-
Sexually transmitted infections such as chlamydia and gonorrhea
-
Prostatitis, which can alter semen composition
These conditions may leave scarring that blocks the sperm pathway. Early diagnosis and antibiotics reduce long?term damage. Fertility Point uses semen analysis, swabs, and imaging to check for infection and inflammation and to plan treatment.
Hormonal Imbalances And Endocrine Disorders
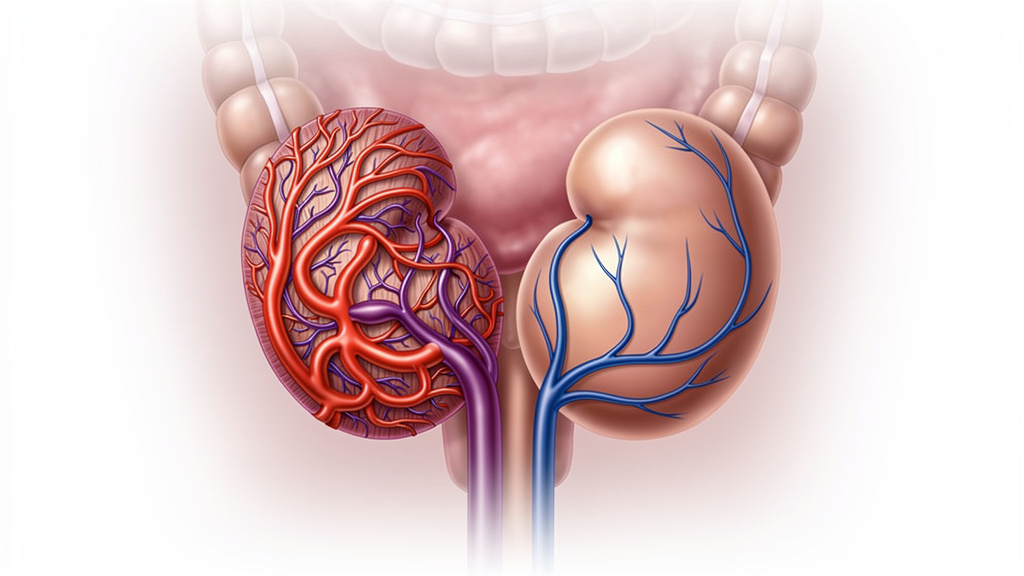
The hypothalamic–pituitary–testicular axis controls sperm production. Signals from the brain stimulate the pituitary gland, which releases FSH and LH to direct the testicles.
Problems in this system can cause:
-
Hypogonadism (low testosterone)
-
High prolactin levels
-
Thyroid disorders
-
Adrenal disorders
Symptoms may include low libido, fatigue, mood changes, or reduced muscle mass. Fertility Point checks full hormone panels and treats imbalances with targeted medicines. External testosterone must be used very carefully, as it can switch off the body’s own sperm production if not managed by a fertility specialist.
Cancer And Cancer Treatments
Cancers of the testicle, prostate, or nearby organs can directly affect fertility. Even cancers elsewhere in the body may impact sperm through:
-
Chemotherapy (damages fast?dividing sperm?producing cells)
-
Radiation therapy, especially to the pelvis
-
Surgery that removes one or both testicles
Some men recover sperm production after treatment; others do not. Because of this, sperm banking before cancer treatment is strongly recommended for men who may want children later. Fertility Point offers urgent fertility preservation so sperm can be frozen quickly, often within days of diagnosis.
Autoimmune Conditions And Anti-Sperm Antibodies
Occasionally the immune system starts to treat sperm as foreign. After trauma, infection, or surgery, some men form anti?sperm antibodies that stick to sperm and interfere with movement or egg binding.
Semen analysis may show clumping or very low motility even when counts are normal. Specialized tests can detect these antibodies. Mild cases may be managed with medication, but IVF with ICSI often provides the most reliable way to bypass the problem.
Sperm-Related Problems: Production, Function, And Quality Issues
Many male infertility reasons come down to issues with:
-
How sperm are produced
-
How well they move
-
Whether they look and function normally
A standard semen analysis measures sperm count, motility, morphology (shape), and semen volume and pH. Fertility Point also uses advanced tests when needed to get a more detailed view.
Azoospermia: Absence Of Sperm In Ejaculate
Azoospermia means no sperm are seen in the semen sample. It can be:
-
Obstructive – sperm are made, but a blockage stops them entering the ejaculate
-
Non?obstructive – the testicles make very few or no mature sperm
Obstructive causes include prior vasectomy, scarring from infections or surgery, or congenital absence of the vas deferens. In many cases, sperm can be collected directly from the epididymis or testicle and used with ICSI.
Non?obstructive azoospermia is often linked to genetic problems, severe hormone issues, or past chemotherapy. A procedure called micro?TESE (microdissection testicular sperm extraction) can sometimes find small pockets of sperm. Fertility Point coordinates micro?TESE with on?site embryology so any sperm found can be frozen and later used for ICSI.
Oligospermia: Low Sperm Count
Oligospermia means a sperm concentration below 15 million per milliliter (WHO reference). The lower the count, the lower the chance of natural conception, although pregnancy is still possible for many couples.
Common causes include:
-
Varicocele
-
Hormone imbalance
-
Smoking, obesity, or poor diet
-
Heat exposure and some medications
-
Genetic conditions
Treatment targets the cause—correcting a varicocele, improving lifestyle, treating hormones, or changing medicines. If counts remain low, IUI (intrauterine insemination) or IVF/ICSI can greatly improve the odds.
Asthenozoospermia: Poor Sperm Motility
Asthenozoospermia refers to poor sperm movement. In a healthy sample, a good share of sperm move forward in a straight line or wide arc (progressive motility). Poor motility can result from:
-
Infections or inflammation
-
Varicocele
-
Oxidative stress
-
Genetic defects in sperm tails
-
Exposure to toxins or anti?sperm antibodies
Treatments may include treating infections, repairing a varicocele, improving lifestyle, and using antioxidant supplements. IUI helps by placing motile sperm closer to the egg, while IVF with ICSI can bypass motility problems altogether.
Teratozoospermia: Abnormal Sperm Morphology
Teratozoospermia means a high percentage of sperm have abnormal shapes. Abnormalities may involve the head, midpiece, or tail and can interfere with swimming and egg penetration.
Labs often use Kruger strict criteria, where even 4% normal forms is considered within the reference range. Many men with low morphology still father children, especially with help.
Causes include genetic factors, varicocele, infections, oxidative stress, and exposure to toxins. Lifestyle changes and antioxidants may help; when morphology stays poor, IVF with ICSI allows embryologists to select the best?appearing sperm under high magnification.
Obstructions And Blockages Preventing Sperm Delivery
Sperm travel from the testicles through the epididymis, vas deferens, ejaculatory ducts, and urethra before leaving the body. A blockage anywhere along this path can cause:
-
Very low semen volume
-
Azoospermia
-
“Dry” ejaculation
Blockages can be present from birth or develop later due to infection, injury, or surgery.
Congenital Causes Of Obstruction
Some men are born without parts of the reproductive tract, especially the vas deferens. This is known as congenital bilateral absence of the vas deferens (CBAVD) and is often linked to changes in the CFTR gene (associated with cystic fibrosis).
Other birth?related problems include cysts or malformations of the ejaculatory ducts and seminal vesicles. Men may have very low semen volume and azoospermia despite normal testicular function.
At Fertility Point, suspected congenital obstruction usually prompts genetic testing and counseling. Instead of complex reconstruction, doctors often collect sperm directly from the testicle or epididymis and use ICSI, which gives good pregnancy rates.
Acquired Obstructions
Acquired blockages arise after:
-
Infections such as epididymitis, urethritis, or prostatitis
-
Trauma to the pelvis or groin
-
Surgery, for example vasectomy, hernia repair, or prostate surgery
Diagnosis involves a physical exam, semen analysis, and imaging such as scrotal or transrectal ultrasound. Fertility Point’s microsurgeons can perform vasectomy reversal or more complex reconnections where appropriate. When surgery is unlikely to help, sperm retrieval combined with IVF/ICSI is often the most direct option.
Ejaculatory Dysfunction
Some men produce sperm but cannot ejaculate normally. Two main patterns are:
-
Retrograde ejaculation – semen flows backward into the bladder
-
Anejaculation – no semen is expelled at all
Causes include diabetes, nerve damage, some medications, spinal cord injury, and surgery near the bladder neck. Treatment might involve medicines, specialized stimulation techniques, or retrieving sperm from urine or the testicles for use in IUI or IVF. Fertility Point matches the method to the cause and the couple’s goals.
Genetic And Chromosomal Causes Of Male Infertility
Genetic factors underlie many of the most severe male infertility cases, particularly azoospermia and very low sperm counts. These can involve:
-
Abnormal chromosome numbers or structures
-
Y?chromosome microdeletions
-
Single?gene mutations
Fertility Point offers comprehensive genetic testing and counseling to explain what these findings mean for treatment and for future children.
Chromosomal Abnormalities
The best?known chromosomal cause is Klinefelter syndrome (47,XXY). Men have an extra X chromosome, which affects testicular development.
Typical features include:
-
Small, firm testicles
-
Low testosterone
-
Azoospermia or severe oligospermia
Many men with Klinefelter now conceive children through micro?TESE and ICSI. Other chromosomal issues, such as translocations or inversions, can impair sperm production or raise the risk of miscarriage. Karyotype testing for both partners may be advised, and preimplantation genetic testing (PGT) can be discussed during IVF.
Y-Chromosome Microdeletions
The Y chromosome carries key genes for sperm production in regions known as AZFa, AZFb, and AZFc. Small missing segments, or microdeletions, are found in about 10–15% of men with azoospermia or severe oligospermia.
-
AZFa or AZFb deletions usually mean a very low chance of finding sperm
-
AZFc deletions often allow some sperm production, with better micro?TESE outcomes
Any male child conceived with sperm carrying a Y microdeletion will inherit the same deletion and likely face similar fertility problems. Fertility Point provides detailed genetic counseling and, when appropriate, discusses PGT or the option of selecting female embryos.
Single Gene Mutations
Changes in single genes can affect fertility in more specific ways. A classic example is the CFTR gene:
-
Men with two disease?causing CFTR mutations usually have cystic fibrosis and almost always lack the vas deferens
-
Men with CBAVD often carry at least one CFTR mutation and may have mild or no lung disease
Because cystic fibrosis is inherited in a recessive pattern, both partners are usually offered CFTR testing. Other gene defects can affect hormone receptors, sperm tail structure, or sperm–egg interaction. IVF with ICSI plus appropriate how genetic testing can often help couples have children while reducing the risk of serious inherited disease.
Lifestyle And Environmental Factors Affecting Male Fertility
Not all male infertility reasons are fixed. Everyday habits and surroundings can have a strong effect on sperm health. The encouraging part is that many of these influences are under our control.
“What is good for your general health is usually good for your fertility.” — Prof. Allan Pacey, Andrologist
Fertility Point integrates lifestyle support—nutrition, exercise, and smoking or substance cessation—into its fertility care.
Diet, Nutrition, And Body Weight

Excess body fat can lower testosterone and reduce sperm production. As BMI rises above 25–30, sperm count and motility often decline. Gradual weight loss usually improves hormone balance and semen parameters over time.
Nutrients that support sperm health include:
-
Antioxidants such as vitamins C and E, selenium, zinc, and folate
-
Omega?3 fatty acids from fish, walnuts, and flaxseed
-
A diet rich in fruits, vegetables, whole grains, nuts, and seeds
Patterns similar to the Mediterranean diet are often linked with better semen quality. Because sperm need about three months to develop, improvements in diet and weight may show up after at least one full sperm production cycle.
Physical Activity And Exercise
Regular, moderate exercise:
-
Improves blood flow
-
Helps with weight control
-
Supports hormone balance
Very intense endurance training or heavy use of hot environments (like long cycling sessions with tight shorts) can have the opposite effect. Fertility Point typically encourages at least 150 minutes of moderate activity per week, along with short movement breaks during long periods of sitting.
Smoking, Alcohol, And Substance Use
Smoking is one of the clearest preventable risks for sperm damage. It increases oxidative stress and is linked with lower counts, weaker motility, and more DNA damage in sperm. Quitting often leads to noticeable improvement within a few months.
Other substances that can impair fertility include:
-
Heavy alcohol intake
-
Marijuana
-
Cocaine and other stimulants
-
Opioids
-
Anabolic steroids (which can shut down sperm production)
Fertility Point discusses these topics without judgment and connects men with support services when needed.
Medications And Supplements
Several medicines can affect sperm, such as:
-
Testosterone replacement therapy (TRT)
-
High?dose anabolic steroids
-
Some ulcer drugs, blood pressure medicines, and chemotherapy agents
Men should never stop prescription drugs on their own. Instead, they should bring a full list of medicines and supplements to their fertility specialist so safer alternatives can be considered where possible.
Environmental And Occupational Exposures
Factors that can harm sperm over time include:
-
Frequent heat exposure (hot tubs, saunas, laptops on the lap, hot work environments)
-
Contact with pesticides, herbicides, solvents, and heavy metals like lead
-
Endocrine?disrupting chemicals such as BPA and some phthalates
Practical steps:
-
Use protective gear at work when exposed to chemicals
-
Keep laptops off the lap and limit hot tub use
-
Choose glass or stainless?steel containers for food and drink
-
Wash fruits and vegetables thoroughly
When occupational risks are high, Fertility Point may coordinate with occupational health experts to protect both fertility and job safety.
Idiopathic Male Infertility: When No Cause Is Found
In some men, tests show abnormal semen or pregnancy does not occur, yet no clear medical, genetic, or lifestyle cause can be identified. This is called idiopathic infertility and may account for 30–50% of male infertility cases.
Not having a clear answer can be frustrating and emotionally draining. But “unexplained” does not mean “untreatable.” It often reflects limitations in current testing rather than an absence of a real problem.
Fertility Point approaches these cases by focusing on what can be improved—general health, oxidative stress, and the use of assisted reproductive techniques that can bypass subtle sperm defects.
The Role Of Oxidative Stress
A major theory in idiopathic infertility is oxidative stress, where reactive oxygen species (ROS) overwhelm the body’s antioxidant defenses. Excess ROS can:
-
Slow sperm motility
-
Distort morphology
-
Damage sperm DNA
Risk factors include smoking, obesity, pollution, varicocele, and chronic infection. Some labs can measure ROS and antioxidant capacity in semen. Treatment often combines lifestyle changes with antioxidant supplements such as vitamins C and E, selenium, zinc, coenzyme Q10, and carnitine.
Treatment Options For Unexplained Infertility
Care usually starts with:
-
Optimizing lifestyle and body weight
-
Treating possible low?grade infections
-
Reviewing medications
-
Adding targeted antioxidant therapy
If pregnancy does not occur, couples may move on to IUI, where a concentrated sperm sample is placed directly into the uterus at ovulation. If several IUIs fail, IVF (with or without ICSI) is usually recommended. During IVF, embryologists can directly observe fertilization and early embryo development, which sometimes reveals issues that basic tests missed.
Fertility Point follows evidence?based pathways, moving stepwise from simpler measures to advanced options while offering counseling and emotional support throughout.
Comprehensive Diagnostic Approaches For Male Infertility
Accurate diagnosis is the foundation of effective treatment. Instead of guessing the cause of male infertility, specialists use a structured evaluation that covers:
-
Medical history
-
Physical examination
-
Semen analysis
-
Hormone testing
-
Imaging and genetic tests when needed
At Fertility Point, each step is explained in plain language so couples understand why each test matters and how it affects the treatment plan.
Medical History And Physical Examination
The doctor will ask about:
-
Childhood issues such as undescended testicles or mumps
-
Past groin or abdominal surgery
-
Chronic diseases (diabetes, thyroid problems)
-
Cancer treatments
-
Current medicines and supplements
-
Sexual function and past pregnancies
The physical exam focuses on the testicles, scrotum, and secondary sexual characteristics, checking for varicocele, small or firm testicles, absence of the vas deferens, breast enlargement, or low body hair. These findings guide which lab and imaging tests are most important.
Semen Analysis: The Cornerstone Test
Semen analysis is the main test for male fertility. After 2–7 days of abstinence, the sample is produced by masturbation and examined within an hour. The lab measures:
|
Parameter |
Normal Reference Value |
|---|---|
|
Volume |
? 1.5 mL |
|
Sperm Concentration |
? 15 million per mL |
|
Total Sperm Number |
? 39 million per ejaculate |
|
Motility |
? 40% motile (32% progressive) |
|
Morphology |
? 4% normal forms (strict) |
|
Vitality |
? 58% live |
Because semen results vary, at least two tests several weeks apart are recommended. Fertility Point uses Computer?Assisted Semen Analysis (CASA) for precise measurements and may add advanced tests such as sperm DNA fragmentation or oxidative stress assessment when needed.
Hormonal Testing
Hormone tests help identify issues in the brain–testicle axis or in other glands. They often include:
-
Total and free testosterone
-
FSH and LH
-
Prolactin
-
Estradiol
-
Thyroid hormones (TSH, free T4)
Patterns in these results point toward primary testicular failure, pituitary or hypothalamic disorders, or medication effects. Fertility Point uses this information to choose appropriate medical therapies or to plan sperm retrieval.
Advanced Diagnostic Testing
When basic tests cannot explain infertility, more specialized studies are used:
-
Scrotal ultrasound for varicocele, tumors, or structural changes
-
Transrectal ultrasound for ejaculatory duct and seminal vesicle problems
-
Genetic tests (karyotype, Y?microdeletions, CFTR mutations)
-
Post?ejaculatory urine analysis for retrograde ejaculation
-
Testicular biopsy, often combined with sperm retrieval, to distinguish obstructive from non?obstructive azoospermia
These investigations provide a more complete picture and help couples choose realistic, informed treatment paths.
Treatment Pathways: From Lifestyle Changes To Advanced Reproductive Technology

Very few couples have no path at all to parenthood. Treatment depends on:
-
The specific male infertility reasons
-
The female partner’s age and fertility
-
How long the couple has been trying
-
Personal preferences and values
Fertility Point offers options ranging from simple lifestyle measures to advanced IVF with ICSI, with clear explanations at each stage.
Lifestyle Optimization And Medical Management
For almost everyone, treatment starts with general health:
-
Reaching a healthier body weight
-
Eating an antioxidant?rich diet
-
Exercising regularly
-
Stopping smoking and limiting alcohol
-
Avoiding heat and toxins where possible
-
Managing stress through counseling or relaxation techniques
Doctors treat infections, adjust medicines that may harm fertility when feasible, and may prescribe antioxidants. Since sperm take around three months to mature, repeat semen analysis after this period often shows how well these steps are working.
Surgical Interventions
Surgery can correct several structural causes:
-
Varicocelectomy for varicocele
-
Vasectomy reversal (vasovasostomy or vasoepididymostomy)
-
TURED (Transurethral Resection of the Ejaculatory Ducts) for ejaculatory duct obstruction
Microsurgical techniques at Fertility Point aim to improve semen quality and, in some cases, restore the possibility of natural conception. Couples weigh these options against sperm retrieval plus IVF/ICSI, especially if the female partner is older or has her own fertility factors.
Sperm Retrieval Techniques
When sperm do not appear in the ejaculate or counts are extremely low, direct sperm retrieval combined with ICSI allows many men to father biological children. Techniques include:
-
PESA (Percutaneous Epididymal Sperm Aspiration)
-
TESA (Testicular Sperm Aspiration)
-
TESE (Testicular Sperm Extraction)
-
Micro?TESE for difficult non?obstructive cases
Even a very small number of sperm can be enough for a full ICSI cycle. Fertility Point coordinates surgical and laboratory teams closely so any retrieved sperm can be examined, frozen, and used at the best possible time.
Conclusion
Male infertility has many possible causes—from varicocele and infections to genetic changes, hormonal problems, lifestyle factors, and oxidative stress. Behind each label is a person or couple coping with worry, disappointment, and uncertainty.
The key message is simple: infertility is a medical condition, not a personal failure. A structured evaluation—with history, examination, semen analysis, hormone and genetic tests, and imaging—turns guesswork into a plan. From there, options open up: lifestyle changes, medicines, surgery, sperm retrieval, and assisted reproduction such as IVF and ICSI.
Fertility Point brings together advanced diagnostics, experienced clinicians, and compassionate support so couples do not have to face this process alone. If you are concerned about male fertility, the most helpful step is to seek a professional assessment rather than waiting in silence. Early action often widens your choices and can bring you closer to the family you hope for.
FAQ's
When should a couple suspect that male infertility might be a problem?
If pregnancy has not occurred after 12 months of regular, unprotected intercourse, both partners should have a fertility evaluation. If the female partner is 35 or older, many experts suggest starting after six months. Men who have had chemotherapy, undescended testicles, major testicular trauma, or very low semen volume should consider testing even earlier at a clinic such as Fertility Point.
Can lifestyle changes alone resolve male infertility?
Sometimes. Men with mild sperm abnormalities linked to weight, smoking, alcohol, or heat exposure may see substantial improvement after several months of healthier habits. However, when there are structural problems, severe hormone issues, or significant genetic factors, lifestyle changes help but are usually male infertility treated. Fertility Point combines lifestyle support with medical, surgical, and IVF?based care when needed.
Is it true that wearing tight underwear causes infertility?
Tight underwear can slightly raise scrotal temperature, which might affect sperm in some men, but it is rarely the only cause of infertility. It is one small part of a much bigger picture. Switching to looser underwear and avoiding extra heat sources (like hot tubs and laptops on the lap) can be helpful, especially when combined with other lifestyle and medical steps.
Does a normal semen analysis guarantee fertility?
No. A normal semen analysis is encouraging but does not guarantee pregnancy. Fertility always involves both partners, and some sperm problems only appear during the fertilization process itself. On the other hand, many men with mildly abnormal semen tests still father children naturally. Fertility Point interprets semen results within the full context of the couple’s health and history.