Top Factors That Affect IVF Success Rates You Should Know
Embarking on the In Vitro Fertilization (IVF) journey is a monumental decision, filled with hope and many questions. One of the most common and critical questions you'll have is: What are the top factors that affect IVF success rates?
The success of IVF isn't determined by a single element; it's a complex interplay of clinical excellence, biological realities, and lifestyle choices. Understanding these factors allows you to manage expectations, make informed decisions, and work proactively with your medical team. We'll explore the key variables that influence your chances and discuss how fertility treatment can be made affordable in Kenya without compromising on quality.
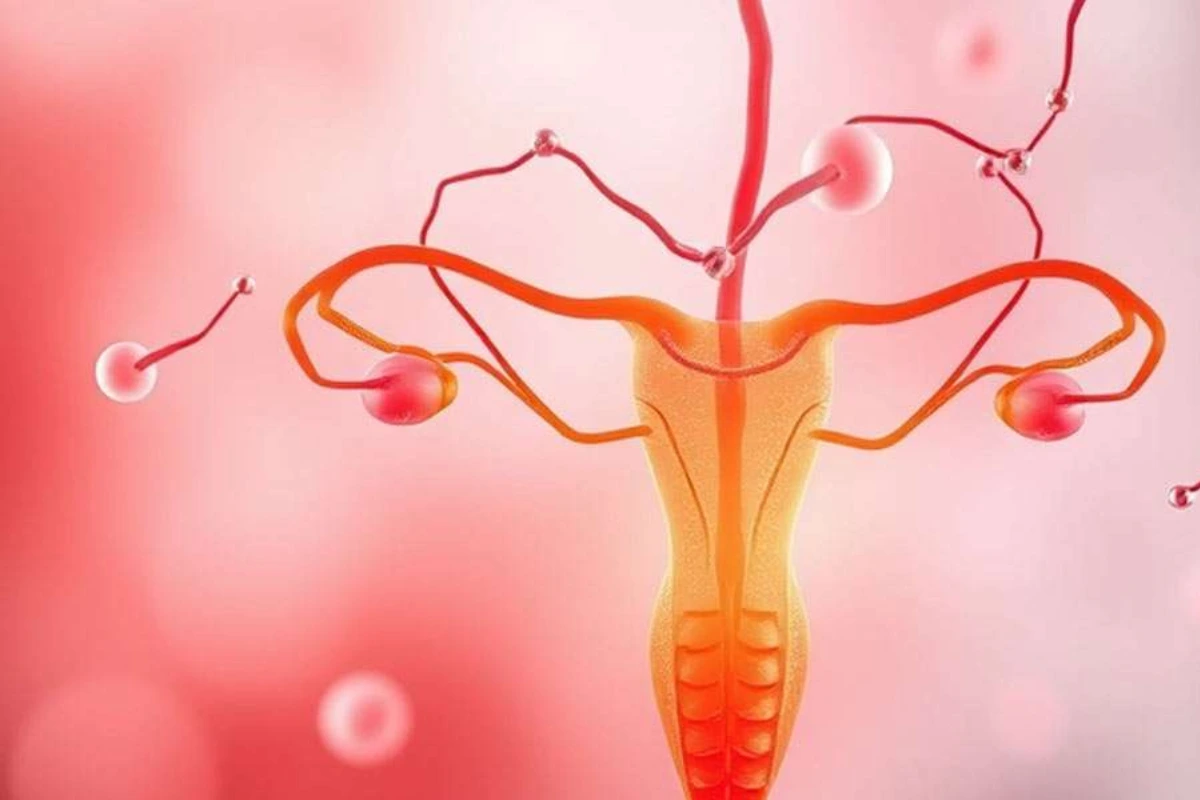
The Overriding Factor: Female Age and Egg Quality
There's no debating the most critical factor influencing IVF success: the age of the woman at the time of egg retrieval. This isn't about general health; it's about the biological quality and quantity of the eggs (ovarian reserve).
Biological Reality
(i) Decline in Quality: As a woman ages, the proportion of eggs with chromosomal abnormalities (aneuploidy) increases significantly. Chromosomally abnormal eggs often fail to fertilize, fail to implant, or result in miscarriage.
(ii) Decline in Quantity: Ovarian reserve—the number of viable eggs remaining—also declines. This is often assessed using blood tests for Anti-Müllerian Hormone (AMH) and an ultrasound check of the Antral Follicle Count (AFC). A low reserve means fewer eggs retrieved, which translates to fewer embryos available for transfer.
| Age Group | Average Live Birth Rate Per Cycle (Approximate) |
| Under 35 | Highest chances, typically over 40-50% |
| 35-37 | Moderate chances, begins to decline (around 30-40%) |
| 38-40 | Significant decline (around 20-30%) |
| Over 40 | Lower chances, typically below 15-20% |
The advantage of a younger age is the higher probability of producing euploid (chromosomally normal) embryos, which are the ones most likely to lead to a successful live birth. If a woman over 40 uses a donor egg from a younger woman, her success rate will align with the donor's age, dramatically illustrating the central role of egg quality.
Embryo Quality and Uterine Receptivity
Even the best eggs and sperm require a conducive environment in the lab and in the uterus. These two factors are critical for the final stage of implantation.
Embryo Quality (The Lab Factor)
After fertilization, the embryo is grown in the lab, ideally to the blastocyst stage (Day 5 or 6). Embryologists assign a grade based on the appearance, growth rate, and cellular structure of the embryo.
(i) Blastocyst Transfer: Transferring an embryo at the blastocyst stage generally yields higher success rates because it allows the embryologist to select the most robust, self-selecting embryos that have survived the first few critical days of development.
(ii) Preimplantation Genetic Testing (PGT): For couples facing advanced maternal age or recurrent miscarriage, PGT (specifically PGT-A for aneuploidy screening) can significantly improve success rates per transfer by ensuring only chromosomally normal embryos are used. This reduces the time and cost spent on failed transfers.
Uterine Receptivity (The Implantation Factor)
The lining of the uterus, known as the endometrium, must be perfectly prepared to receive the embryo.
(i) Endometrial Thickness: The ideal thickness for a successful transfer is generally considered to be $\ge 7\text{mm}$. A lining that is too thin or too thick, or displays an irregular pattern, can lead to implantation failure.
(ii) Uterine Health: Conditions like uterine fibroids (especially those growing into the cavity), endometriosis, adhesions (scar tissue), or polyps can cause chronic inflammation or structural issues that interfere with implantation. Addressing these issues (often via hysteroscopy) before transfer is essential.
The Nature of Infertility and Duration
The underlying cause of infertility dictates the most effective treatment protocol and influences the outcome.
Primary Infertility Factors
(i) Tubal Factor: Blocked or damaged fallopian tubes (e.g., due to previous infection like PID) often have excellent success rates with IVF, as the procedure effectively bypasses the damaged structures.
(ii) Male Factor: Severe male factor infertility (low count, poor motility, etc.) is successfully overcome by ICSI (Intracytoplasmic Sperm Injection), which is typically performed as part of the IVF cycle.
(iii) Ovarian Dysfunction: Issues like Polycystic Ovary Syndrome (PCOS) can be complex but often respond well to controlled ovarian stimulation, though sometimes requiring specialized protocols to mitigate the risk of Ovarian Hyperstimulation Syndrome (OHSS).
(iv) Unexplained Infertility: When all tests are normal, IVF provides the most effective diagnostic and therapeutic solution, often yielding success rates, as the egg and sperm quality are often intrinsically sound.
Duration and Previous Attempts
Couples who have been trying to conceive for a very long duration (e.g., over 8 years) or who have had multiple previous failed IVF cycles may have a lower prognosis due to factors that have not yet been fully identified or addressed.
Clinic Expertise and Laboratory Environment
The clinic you choose plays a massive role in your success. The results aren't just about the patient; they are about the quality of the technology, the skill of the staff, and the protocols used.
The Role of the IVF Centre
(i) Embryology Lab Quality: The IVF laboratory must maintain stringent standards for temperature, air quality, culture media, and equipment. The best IVF centers in Kenya invest heavily in state-of-the-art labs because the embryos spend their first, most vulnerable days there.
(ii) Embryologist Skill: The embryologist's expertise in handling gametes, performing ICSI, grading embryos, and executing the delicate process of vitrification (embryo freezing) and thawing is paramount.
(iii) Doctor's Protocol: The fertility specialist’s ability to customize the ovarian stimulation protocol (medication type and dosage) and ensure the correct timing of the egg retrieval is critical for maximizing the number of high-quality eggs.
Fertility Point, as one of the best IVF centres in Kenya, emphasizes a combination of advanced technology and deeply personalized protocols to address each patient's unique needs, understanding that the clinical environment is a core driver of successful outcomes.
Lifestyle and Underlying Health Conditions
Your personal health is a factor that you have the power to influence and control. Making positive changes can directly enhance the quality of your gametes and improve uterine receptivity.
Lifestyle Factors
| Factor | Impact on IVF Success |
| Body Mass Index (BMI) | Women who are significantly overweight (high BMI) or underweight (low BMI) can experience hormonal imbalances that affect egg quality, response to medication, and implantation rates. Optimizing BMI can improve success. |
| Smoking/Nicotine | Smoking severely impairs egg and sperm quality, reduces ovarian reserve, and lowers the chance of implantation. Quitting smoking is mandatory. |
| Alcohol/Caffeine | Excessive alcohol and high caffeine intake can negatively affect fertility and should be minimized or eliminated during treatment. |
| Stress | While not a direct cause of IVF failure, chronic stress can negatively impact adherence to treatment and overall well-being. Stress management techniques are highly recommended. |
Medical Factors
Uncontrolled medical issues can reduce success. These include diabetes, thyroid dysfunction (hypo- or hyperthyroidism), and certain autoimmune disorders. Ensuring these conditions are managed by a specialist before and during the IVF cycle is crucial.
How Fertility Treatment Can Be Made Affordable in Kenya
The high cost of IVF is a major barrier for many couples seeking treatment in Kenya, where a single cycle can often be equivalent to a year's average income. Addressing the question of how fertility treatment can be made affordable in Kenya requires innovative approaches from both clinics and financial institutions.
Strategies for Affordability
-
Package Deals for Multiple Cycles: Since most couples require two or three cycles for a successful live birth, clinics can offer discounted packages for 2 or 3 attempts. This reduces the risk of having to pay full price for multiple cycles.
-
Use of Frozen Embryo Transfer (FET): A single, successful fresh retrieval cycle that yields multiple embryos allows subsequent attempts (FETs) to be significantly cheaper than a full fresh cycle, as they eliminate the cost of medication and egg retrieval. Utilizing a Freeze-All approach maximizes the cost-efficiency of the initial retrieval.
-
Flexible Financing and Payment Plans: Partnerships with local banks or lending institutions to offer low-interest medical loans specifically for fertility treatments can ease the immediate financial burden. Clinics can also offer in-house installment plans.
-
Government and Corporate Subsidies: The long-term goal for IVF centers in Kenya is to lobby for government support or the inclusion of IVF in national health insurance schemes. Additionally, some progressive private companies are starting to offer fertility benefits to their employees, similar to developed nations.
-
Cost-Effective Protocols: Utilizing milder stimulation protocols or natural cycle IVF (when appropriate) can significantly reduce the cost of medications, which are a major expense in the cycle.
By embracing these strategies, the best IVF centres in Kenya, like Fertility Point can work towards making parenthood more accessible to the wider population.
Top 10 Best IVF Centres in Kenya
Choosing a clinic with demonstrated success, ethical practices, and advanced technology is vital. Here are some of the most recognized and high-performing ivf centers in kenya:
-
Fertility Point
-
Harley Street Fertility Centre Kenya (HSFC KE)
-
Nairobi IVF Centre
-
Victoria IVF & Fertility Centre
-
Mediheal Diagnostic & Fertility Centre
-
Kenya IVF and Fertility Research Centre
-
Aga Khan University Hospital Fertility Clinic
-
LifeBridge Fertility Clinic
-
Footsteps to Fertility Centre
-
The Nairobi Fertility Center
The reputation and success rates of a Fertility Clinic should always be evaluated alongside its commitment to transparency and patient support.
Summary: Your Proactive Role in IVF Success
Your IVF success rate is a product of factors you can and cannot control. While you cannot change your age, you can choose the best Fertility Clinic, optimize your lifestyle, and undergo pre-treatment procedures (like PGT or hysteroscopy) to address underlying issues.
The dedication of the expert team at Fertility Point to advanced lab work, personalized protocols, and ethical transparency is designed to maximize the influence of the positive factors while mitigating the risks of the negative ones. By understanding the top factors that affect IVF success rates, you become an empowered and proactive partner in your journey toward parenthood.
FAQ's
What is the most important factor affecting IVF success?
The most critical factor is the woman’s age, as egg quality and quantity naturally decline with time, directly impacting embryo development and implantation.
Can IVF success rates improve with lifestyle changes?
Yes. Maintaining a healthy BMI, avoiding smoking and alcohol, managing stress, and controlling medical conditions like thyroid issues or diabetes can significantly improve IVF outcomes.
How does embryo quality influence IVF success?
High-quality embryos, especially blastocysts, have a better chance of implanting and leading to a successful pregnancy. Techniques like PGT-A can help select the healthiest embryos.
What conditions can reduce IVF success rates?
Uterine issues like fibroids, polyps, endometriosis, thin endometrium, hormonal imbalances, chronic medical conditions, and poor sperm parameters can affect results.