What Are the Options for Couples With Low Ovarian Reserve?
Embarking on the journey to parenthood when facing a diagnosis of Low Ovarian Reserve can feel daunting. It’s natural to experience a mix of frustration, anxiety, and a profound sense of urgency. The term Low Ovarian Reserve simply means that a woman has fewer eggs remaining in her ovaries, or that the quality of those remaining eggs may be lower, compared to other women her age. It's a key factor in female fertility that can significantly impact the chances of conceiving naturally. However, thanks to continuous advancements in reproductive medicine, several promising options are available for couples with Low Ovarian Reserve to help them achieve their dream of having a baby.
The key to navigating this challenge is to seek an early and comprehensive evaluation with an experienced fertility specialist. A personalized and evidence-based treatment plan is paramount, as what works for one couple may not be the optimal path for another. The ultimate goal is to find the most effective and efficient route to a successful pregnancy.
Understanding Low Ovarian Reserve: The Foundation of the Challenge
To appreciate the treatment options, it’s helpful to understand the biology of Low Ovarian Reserve. Women are born with a finite number of eggs. This quantity, known as the ovarian reserve, naturally declines over time. Various factors, including genetics, prior ovarian surgery, endometriosis, smoking, and certain medical treatments like chemotherapy or radiation, can accelerate the rate of decline.
Diagnosis typically involves blood tests for Anti-Müllerian Hormone (AMH)—which correlates well with the number of remaining eggs—and Follicle-Stimulating Hormone (FSH) and estradiol measured early in the menstrual cycle. A transvaginal ultrasound to determine the Antral Follicle Count (AFC) also provides a crucial snapshot of the current ovarian reserve. The combination of low AMH, high FSH, and a low AFC a strong indicator of Low Ovarian Reserve.
What Are the Options for Couples With Low Ovarian Reserve?
The treatment path for couples with Low Ovarian Reserve generally falls into two main categories: using the woman's own eggs or using donor eggs. The choice depends heavily on the woman's age, the severity of the reserve depletion, previous treatment history, and, critically, the couple's personal preferences and desire for a genetic link to the child.
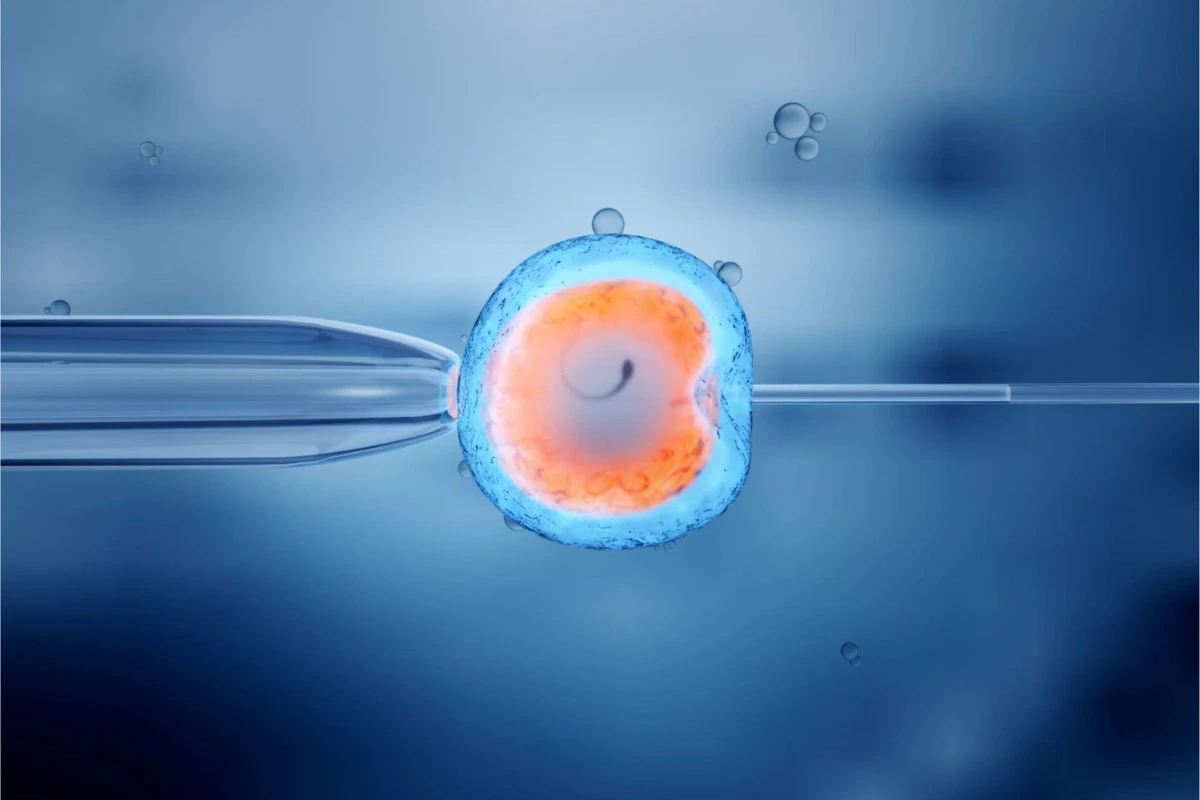
Option 1: In Vitro Fertilization (IVF) with the Patient’s Own Eggs
For many couples with Low Ovarian Reserve, In Vitro Fertilization (IVF) remains the first and most viable option using the woman's genetic material. The challenge here is the typically poor response to standard ovarian stimulation, often resulting in fewer eggs retrieved. However, specific protocols and adjuvant therapies can be employed to maximize the chances.
A. Customized Ovarian Stimulation Protocols
Fertility specialists have developed specialized IVF Treatment in Kenya protocols tailored for patients with diminished reserve:
1. Mild Stimulation IVF: This approach uses lower doses of fertility medication, often in combination with oral agents like Clomiphene Citrate or Letrozole. The goal is to collect fewer, but potentially higher-quality eggs, minimizing medication costs and the risk of Ovarian Hyperstimulation Syndrome (OHSS), which is rare in this population but always a concern.
(i) Advantage: Lower medication dosage, shorter cycle time, potentially better egg quality.
(ii) Disadvantage: Lower egg yield per cycle, requiring multiple cycles to accumulate a sufficient number of embryos.
2. Conventional High-Dose Stimulation: While earlier studies suggested high doses of gonadotropins might yield more eggs, current consensus often favors a more measured approach. However, for some women with moderate DOR, higher doses may be considered, often with a Gonadotropin-Releasing Hormone (GnRH) Antagonist protocol to prevent premature ovulation.
(i) Advantage: Attempts to maximize the number of eggs in a single cycle.
(ii) Disadvantage: High medication cost, may not significantly improve egg yield or quality over mild stimulation.
3. Natural Cycle or Modified Natural Cycle IVF: This protocol involves minimal or no stimulation, allowing the one dominant, naturally-selected follicle to mature. The modified cycle may use a small dose of medication or an antagonist to fine-tune the timing.
(i) Advantage: Extremely low medication cost, no risk of OHSS, focuses on the "best" natural egg.
(ii) Disadvantage: Very low egg yield (often just one), high cycle cancellation rate, very low overall cumulative success rate per transfer.
4. Luteal Phase Stimulation (or "Double Stimulation"): Also known as DuoStim, this relatively newer protocol involves two separate stimulation and egg retrieval procedures within the same menstrual cycle—one in the follicular phase and one immediately following in the luteal phase. This can be particularly effective for women who are poor responders.
(i) Advantage: Significantly increases the number of eggs and embryos accumulated in a short period, effectively saving time.
(ii) Disadvantage: Requires two procedures, can be more physically demanding and costly than a single cycle.
B. Adjunctive Therapies and Supplements
Various supplements are frequently recommended to help improve egg quality in the months leading up to an IVF cycle, as it takes approximately three months for a follicle to mature. These are not a cure for Low Ovarian Reserve but aim to optimize the cellular environment:
(i) Coenzyme Q10 (CoQ10): A potent antioxidant believed to improve mitochondrial function in the egg, potentially enhancing egg quality and embryo development.
(ii) Dehydroepiandrosterone (DHEA): A mild androgen supplement that, for some women with DOR, may improve ovarian response and pregnancy rates, though its use remains debated and should be monitored by a doctor.
(iii) Melatonin, Myo-Inositol, and Omega-3 Fatty Acids: These supplements are also often included in pre-treatment regimens to support egg health.
C. Embryo Accumulation and Pre-implantation Genetic Testing (PGT)
Because the success of IVF for couples with Low Ovarian Reserve is primarily driven by securing a euploid (genetically normal) embryo, specialists often recommend:
-
Embryo Banking (Accumulation): Instead of proceeding to transfer after a single retrieval that yields few embryos, a couple may undergo multiple IVF cycles to freeze and accumulate a cohort of embryos. This increases the chance of having a euploid embryo for transfer.
-
Pre-implantation Genetic Testing for Aneuploidy (PGT-A): As egg quality diminishes with Low Ovarian Reserve, the risk of chromosomal abnormalities (aneuploidy) in the resulting embryos increases. PGT-A allows the specialist to screen the embryos and select only the one(s) confirmed to be euploid, significantly increasing the success rate per embryo transfer and reducing the risk of miscarriage.
Option 2: IVF with Donor Eggs
When the ovarian reserve is severely depleted, or when multiple cycles with the patient’s own eggs have failed, IVF with donor eggs often represents the highest probability of a successful pregnancy. This is a profound and intensely personal decision for couples with Low Ovarian Reserve, as it means the resulting child will not be genetically related to the female partner.
The donor egg is fertilized with the male partner’s sperm (or donor sperm, if needed) in the laboratory. The resulting embryo is then transferred into the recipient woman's uterus, allowing her to carry and give birth to the baby.
(i) Advantage: Exceptionally high success rates (often 50-70% per transfer, depending on the age of the donor), short path to pregnancy.
(ii) Disadvantage: Loss of genetic link for the female partner, psychological and emotional adjustment, and generally higher cost.
In a country like Kenya, IVF in Kenya utilizing a donor program may involve both local and international donors, offering a wider choice pool, though ethical and legal considerations must always be paramount. Fertility Point and other reputable clinics provide comprehensive counseling to help couples navigate this important decision.
Option 3: Natural Conception and Minimal Intervention
For some couples with Low Ovarian Reserve, particularly those with low but still detectable ovarian function and whose main fertility issue is not blocked tubes or severe male factor infertility, attempting to conceive naturally or with minimal assistance, like Timed Intercourse or Intrauterine Insemination (IUI), may still be explored. Given that only one good-quality egg is needed, and despite the low odds, some couples prefer to continue trying naturally while pursuing lifestyle modifications that may subtly influence egg quality.
(i) Advantage: Zero invasiveness, no medical costs, chance to conceive naturally.
?
(ii) Disadvantage: Very low chance of success, significant time delay.
Top 10 Fertility Clinics in Kenya: A Resource for Hope
Seeking advanced fertility care, especially for a complex issue like Low Ovarian Reserve, requires a center with expertise, advanced technology, and compassionate care. Here is a list of prominent centers offering quality IVF
Treatment in Kenya:
-
Fertility Point
-
Nairobi IVF Centre
-
Harley Street Fertility Centre, Kenya
-
Kenya IVF and Surrogacy Centre
-
Victoria IVF & Fertility Centre
-
The Nairobi Hospital Fertility Centre
-
Aga Khan University Hospital Fertility Clinic
-
Kijabe Hospital Assisted Reproduction Unit
-
Medicover Fertility, Nairobi
-
Eldoret Hospital IVF Centre
Summary: A Journey of Hope and Customization
For couples with Low Ovarian Reserve, the path to parenthood is one of informed decision-making and resilience. It is crucial to remember that while the quantity of eggs is reduced, all hope is not lost, as it only takes one healthy embryo to achieve a successful pregnancy. Whether a couple chooses to pursue an aggressive protocol like DuoStim and PGT-A with their own eggs, or finds peace and a higher chance of success through donor eggs, a clear, personalized treatment strategy is essential.
Consulting with experts at a specialized Fertility Clinic like Fertility Point ensures that every available option is explored with the highest standards of care and technology. The most successful outcomes are almost always a result of a strong partnership between the couple and their dedicated medical team.
FAQ's
Can lifestyle changes improve my ovarian reserve?
No, you cannot increase the total number of eggs in your ovarian reserve, as women are born with their lifetime supply. However, lifestyle changes can potentially improve the quality of the remaining eggs. Maintaining a healthy diet (rich in antioxidants), engaging in moderate exercise, and eliminating smoking and excessive alcohol are critical steps. Supplements like CoQ10 are often recommended to optimize egg health in the three months leading up to retrieval.
Is IVF with my own eggs worth attempting if my AMH is very low (e.g., below 0.5 ng/mL)?
This is a highly personalized decision. While a very low AMH indicates a significantly reduced chance, it does not mean zero chance. If the female partner is relatively young (under 38), a few cycles using a mild or double stimulation protocol to "bank" a few embryos for PGT-A screening may be a worthwhile approach. However, if the woman is older or has failed multiple cycles, the chance of success with donor eggs is substantially higher and should be seriously considered to conserve time, money, and emotional energy.
What are the main disadvantages of using donor eggs?
The primary disadvantage is the lack of a genetic link between the female partner and the child. This requires careful emotional preparation and counseling. Other disadvantages include the higher total cost associated with donor compensation and agency fees, and the potential long waiting time to find a suitable donor, depending on the program and location.
How many cycles of IVF should we attempt before considering donor eggs?
There is no set number, but a common clinical metric is the number of retrieved eggs or euploid embryos accumulated. If a couple has undergone 2-3 full-dose or customized cycles without retrieving enough eggs (e.g., fewer than five to seven in total) or without achieving a single euploid embryo, a pivot to donor eggs or other options is often recommended. A full discussion with your specialist at a Fertility Clinic like Fertility Point is necessary to set realistic goals.