What Is ICSI and How Does It Differ From IVF?
Dealing with infertility can feel like navigating a complex maze. When you hear terms like IVF and ICSI, it's natural to feel overwhelmed. You might be wondering, "What is ICSI and How Does It Differ From IVF?" You're not alone. Many couples on their journey to parenthood face the same questions.
The good news is that both are highly advanced, proven forms of Assisted Reproductive Technology (ART) that offer incredible hope. While In Vitro Fertilization (IVF) is the foundational procedure, Intracytoplasmic Sperm Injection (ICSI) is a specialized technique performed as a part of the IVF process.
Let's break down exactly what each procedure entails, how they differ, why a doctor might recommend one over the other, and what your journey might look like, particularly when seeking ICSI Treatment in Kenya or IVF Treatment in Kenya. Understanding these details will help you feel more informed and empowered as you take the next steps toward building your family.
What Is IVF? The Foundation of Assisted Reproduction
In Vitro Fertilization, or IVF, translates literally to "fertilization in glass." It is the most common and well-known type of ART. The basic principle of IVF is to manually combine an egg and sperm in a laboratory dish.
The IVF Process: Step-by-Step
The IVF process is a structured, multi-step journey designed to maximize the chance of a successful pregnancy.
1. Ovarian Stimulation: The cycle begins with the female partner taking fertility medications for about 8 to 14 days. These medications, which often involve daily injections of Follicle-Stimulating Hormone (FSH), stimulate the ovaries to produce multiple eggs, rather than the single egg normally released during a natural cycle. The goal is to collect several healthy eggs to increase the chances of a successful outcome.
2. Monitoring: Throughout the stimulation phase, the woman's progress is carefully monitored. The fertility specialist uses regular ultrasound scans to check the growth of the egg-containing follicles and blood tests to monitor hormone levels. This monitoring is crucial for timing the next steps precisely and for adjusting medication dosages.
3. The "Trigger Shot": Once the follicles reach a mature size, a final hormone injection, often called the "trigger shot" (usually hCG), is administered. This shot prompts the eggs to undergo final maturation and prepares them for retrieval. It is timed very precisely, typically 35 to 36 hours before the egg retrieval procedure.
4. Egg Retrieval: This is a minor surgical procedure performed under light sedation. The fertility specialist uses a thin needle, guided by ultrasound, to gently aspirate the fluid from the follicles and collect the mature eggs from the ovaries. The procedure typically takes about 20 to 30 minutes. Simultaneously, the male partner provides a fresh semen sample.
5. Traditional Fertilization (Insemination): This is the step that defines traditional IVF. The collected eggs are placed in a special culture dish with tens of thousands of processed, healthy, motile sperm. The sperm are then left to fertilize the eggs naturally, mimicking the natural conception process, but outside the body. It’s up to one of the sperm to penetrate the egg’s outer layer on its own.
6. Embryo Culture: The fertilized eggs (now called embryos) are carefully monitored in the laboratory for several days as they grow and divide. The embryologists look for signs of healthy development, often allowing them to grow to the blastocyst stage (day 5 or 6).
7. Embryo Transfer: The highest-quality embryo(s) are selected and gently transferred into the woman's uterus using a soft, thin catheter. This procedure is quick, usually painless, and does not require anesthesia.
8. Pregnancy Test: About 10 to 14 days after the embryo transfer, a blood test is performed to determine if implantation has occurred and if the patient is pregnant.
What Is ICSI? The Precision Intervention
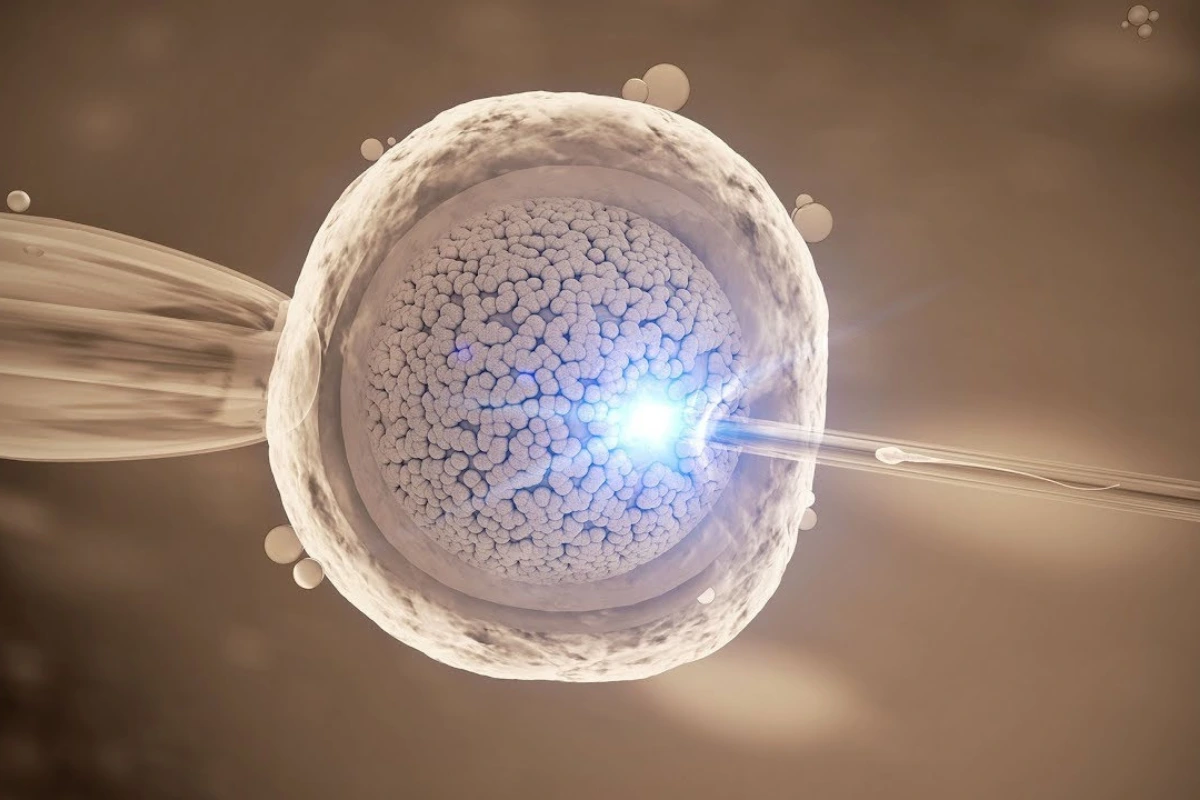
ICSI, or Intracytoplasmic Sperm Injection, is a specialized and highly effective variation of IVF. The main difference lies in the fertilization step.
The core process of ovarian stimulation, egg retrieval, embryo culture, and embryo transfer remains the same as standard IVF. However, when it comes to combining the egg and sperm, the approach is fundamentally different.
The ICSI Fertilization Process
Instead of placing thousands of sperm with the egg and allowing one to penetrate naturally (as in traditional IVF), the embryologist takes direct control.
-
Sperm Selection: A single, healthy-looking sperm is carefully selected by a skilled embryologist under a high-powered microscope.
-
Direct Injection: Using an extremely fine glass needle (a micropipette), a single sperm is gently but deliberately injected directly into the center, or cytoplasm, of the mature egg. This action entirely bypasses the need for the sperm to navigate and penetrate the egg's outer layers on its own.
-
Fertilization Check: Like in IVF, the injected eggs are then placed in an incubator and checked about 16-18 hours later to see if successful fertilization has occurred.
The use of ICSI is a significant breakthrough in fertility treatment, offering a solution for many couples who previously had limited options. For those considering ICSI Treatment in Kenya, it’s a standard, well-established procedure offered at top centers.
How Does ICSI Differ From IVF?
The distinction between ICSI and traditional IVF is specific but profound, revolving entirely around the method of fertilization.
| Feature | Traditional IVF (In Vitro Fertilization) | ICSI (Intracytoplasmic Sperm Injection) |
| Method of Fertilization | Passive/Natural selection: Many sperm are placed in a dish with the egg, and one sperm must fertilize it on its own | Active/Direct injection: A single, selected sperm is injected directly into the center (cytoplasm) of the egg |
| Indication/Recommendation | Generally used for tubal factor infertility, ovulation issues, or unexplained infertility (where male factor is not severe) | Primarily used for severe male factor infertility (low count, poor motility, abnormal shape), previous poor/failed fertilization with IVF, or use of surgically retrieved sperm. |
| Level of Intervention | Less invasive in the fertilization stage | More invasive, requiring a skilled embryologist to handle the egg and sperm directly. |
| Cost | Typically, slightly lower than an ICSI cycle, as it requires less intense lab work | Often slightly higher than traditional IVF due to the specialized equipment and the high level of skill required for the micromanipulation technique. |
In simple terms, ICSI is a powerful tool used within an IVF cycle. When a couple is undergoing an IVF cycle, the decision is made at the fertilization stage whether to use the traditional method or to employ the precision of ICSI.
When Is ICSI Recommended? The Key Indications
The decision to use ICSI is generally based on specific diagnostic criteria, particularly concerning the male partner's fertility profile. Your doctor at a facility like Fertility Point will review all test results before making a recommendation.
Primary Indications for ICSI
The technique was developed primarily to overcome severe male factor infertility, making it a game-changer for many couples. Indications include:
(i) Oligozoospermia (Low Sperm Count): When the concentration of sperm in the ejaculate is too low, the chances of natural penetration in a dish are minimal.
(ii) Asthenozoospermia (Poor Sperm Motility): If the sperm are unable to swim effectively, they won't reach and penetrate the egg on their own. ICSI bypasses this mobility issue entirely.
(iii) Teratozoospermia (Abnormal Sperm Morphology): When a high percentage of sperm have an abnormal shape, this can prevent them from penetrating the egg.
(iv) Surgically Retrieved Sperm: If sperm must be retrieved directly from the testes or epididymis (via procedures like TESA, TESE, or PESA) due to blockages (e.g., following a vasectomy) or a complete absence of sperm in the ejaculate (Azoospermia). Surgically retrieved sperm cannot often fertilize an egg naturally.
(v) Previous Fertilization Failure: If a couple has undergone a previous standard IVF cycle where few or none of the eggs were fertilized, ICSI is typically recommended for the next attempt.
(vi) Using Frozen Eggs (Oocyte Vitrification): The freezing process can sometimes slightly harden the outer layer of the egg, and ICSI ensures successful penetration.
(vii) Preimplantation Genetic Testing (PGT): In cases where the embryo will undergo genetic testing, ICSI is sometimes preferred to ensure that only a single sperm is used, preventing extraneous sperm DNA from interfering with the test results.
In cases of unexplained infertility or when a small number of eggs are retrieved, some clinics may also opt for ICSI to maximize the fertilization rate, although this use is sometimes debated among specialists. For couples seeking ICSI Treatment in Kenya, these are the common clinical scenarios where the procedure is employed.
Advantages and Disadvantages of ICSI
Like any medical procedure, ICSI has both significant benefits and potential drawbacks that you and your partner should carefully discuss with your fertility specialist.
Advantages of ICSI
-
Overcomes Severe Male Infertility: This is the most crucial benefit. ICSI provides a viable path to biological parenthood for men with very low sperm counts, poor motility, or morphological issues, where traditional IVF would likely fail.
-
High Fertilization Rate: For couples with male factor issues, ICSI generally achieves a higher fertilization rate (the percentage of eggs that successfully fertilize) than traditional IVF, often between 50% and 80%.
-
Use of Surgically Retrieved Sperm: It is the only way to achieve fertilization using sperm retrieved directly from the male reproductive organs.
-
A Solution for Previous Failures: It offers a successful alternative for couples who have experienced total or partial fertilization failure with standard IVF.
Disadvantages and Risks of ICSI
-
Slightly Higher Risk of Egg Damage: There is a minimal risk that the egg may be damaged during the injection process by the micropipette, though this is rare in the hands of a skilled embryologist.
-
Does Not Guarantee Embryo Development: While ICSI ensures fertilization (the sperm enters the egg), it does not guarantee that the resulting embryo will be of high quality or that it will successfully implant in the uterus. Fertilization is only the first step.
-
Potential for Inheriting Male Infertility: In cases where the male infertility is due to a genetic issue, there is a small theoretical risk that a male child conceived through ICSI may inherit the same fertility issue. Genetic counseling is highly recommended in such cases.
-
Slightly Increased Risk of Birth Defects: While overall ART is very safe, some studies have shown a small, marginal increase in certain rare congenital conditions (such as specific genetic syndromes or hypospadias) in children conceived via ICSI. However, experts suggest that this increased risk may be linked to the underlying cause of infertility (the quality of the sperm) rather than the ICSI procedure itself. The absolute risk remains very low.
-
Increased Cost: Due to the need for specialized equipment and the precise, time-consuming nature of the micromanipulation, an ICSI cycle generally costs more than a traditional IVF cycle. When researching IVF Treatment in Kenya, make sure to inquire about the additional cost for ICSI.
The Journey to Parenthood: IVF and ICSI in Kenya
The field of reproductive medicine has seen remarkable growth in East Africa, offering world-class care right here at home. For couples exploring fertility options, seeking IVF Treatment in Kenya or ICSI Treatment in Kenya means having access to advanced technology and experienced specialists.
Choosing the right clinic is perhaps the most important decision you will make. You want a team that not only offers state-of-the-art technology but also provides compassionate, personalized care.
When you are ready to explore your options, scheduling a consultation at a reputable Fertility Clinic like Fertility Point is the first and most critical step. Their specialists can guide you through the initial testing, provide an accurate diagnosis, and recommend whether standard IVF or the specialized ICSI procedure is the best path for your unique situation.
Summary: A Path Forward
The question of "What Is ICSI and How Does It Differ From IVF?" ultimately comes down to the mechanics of fertilization.
-
IVF is the overarching procedure where eggs and sperm are combined outside the body.
-
ICSI is a micro-tool within IVF where a single sperm is actively injected into the egg, specifically used to overcome challenges like severe male factor infertility.
Both are powerful forms of Assisted Reproductive Technology designed to help couples achieve their dream of parenthood. The journey requires patience, information, and a strong partnership with your medical team. By choosing a dedicated and experienced center, such as the Fertility Clinic team at Fertility Point, you ensure you are receiving expert guidance and the most suitable treatment, whether that is ICSI Treatment in Kenya or standard IVF Treatment in Kenya. Take that first step with confidence—the future of your family is in good hands.
FAQ's
What is the difference between IVF and ICSI?
The main difference lies in how fertilization occurs. In IVF, multiple sperm are placed with an egg, and one fertilizes it naturally. In ICSI, a single sperm is directly injected into the egg’s cytoplasm, making it ideal for cases of male infertility or previous IVF failure.
When is ICSI recommended over IVF?
ICSI is usually recommended for severe male factor infertility, such as low sperm count, poor motility, or abnormal sperm shape. It’s also used when sperm are retrieved surgically, when using frozen eggs, or after failed IVF attempts.
Is ICSI more successful than IVF?
ICSI often leads to higher fertilization rates in cases of male infertility, but pregnancy rates are similar to IVF when sperm quality is normal. Success depends on several factors, including egg quality, embryo development, and the woman’s age.
How safe is the ICSI procedure?
ICSI is considered safe and has been used for decades. However, there is a small risk of egg damage during injection and a minimal increase in certain rare genetic conditions. Genetic counseling is recommended if the male infertility is hereditary.